Psoriasis is a skin condition where new skin forms at a faster rate, showing up as red rashes with whitish scales, commonly over elbows, knees, and other body parts. It may sometimes involve nails and joints. It affects up to 2% of the global population. Nowadays it is considered a lifestyle disorder.
It is not a life-threatening disease, but recurrences are common.
It is a disease which is treatable and can be effectively and well controlled.
Psoriasis is not an infectious disease, and cannot be transmitted by contact such as touch, or sharing clothes and food.
It is not a rule that children of affected parents will develop psoriasis. However, there is a slightly higher chance of developing psoriasis compared to children of non-affected parents.
Psoriasis can affect anyone, at any age.

Many people who get psoriasis have it for variable duration, with periods of flares and remissions.
It is advisable to visit IADVL dermatologist.
Mostpatients have flares which are triggered during periods of lowimmunity, and it is best to keep immune system robust and healthy atall times, with a healthy lifestyle.
Psoriasis is well treatable.
Yes, psoriasis can recur in some individuals. Each recurrence should be shown to treating dermatologist, who will prescribe a suitable treatment regimen after examining.
A person with psoriasis can marry and have children.
Regular exercise, getting fresh air and sunlight
Dietary modification: Consume fresh seasonal fruits and nutritious, protein rich food. Avoid high glycaemic index foods and junk, processed items.
Stop smoking.
Avoid/ limit intake of alcohol
Getting adequate sleep daily, around 7-9 hours of continuous sleep, and maintaining body’s circadian rhythm.
Practice meditation/ yoga/ breathing exercises to reduce stress
There is no need to supplement with multivitamins/ protein powders/ resort to online purchases without consulting your dermatologist.
Always keep your doctor informed about treatment progress, and do timely follow-ups; inform when rashes increase.
Physical trauma (injury, scratches, shaving, tattoo, piercing)
Mental or physical stress
Infections (psoriasis can flare up after sore throat, ear infection, bronchitis or any other infections, including viral flu/ influenza/COVID)
Certain medications. (Always take opinion of your dermatologist before starting any medications)
Drinking alcohol frequently or in excess
Smoking
Dry and cold weather/ seasonal variations
Low/ weakened immunity and not taking care of balanced diet and lifestyle.
Learning (and avoiding) what triggers your psoriasis
Sticking to a good psoriasis skin care routine. Always consult for dermatologist on appropriate use of emollients and medications.
Living a healthy lifestyle
Using medication when necessary
It may affect other organs such as joints, and nails. If there is joint pain, inform your treating doctor. Multi-disciplinary team including rheumatologists are needed to handle some patients, for better treatment and recovery.
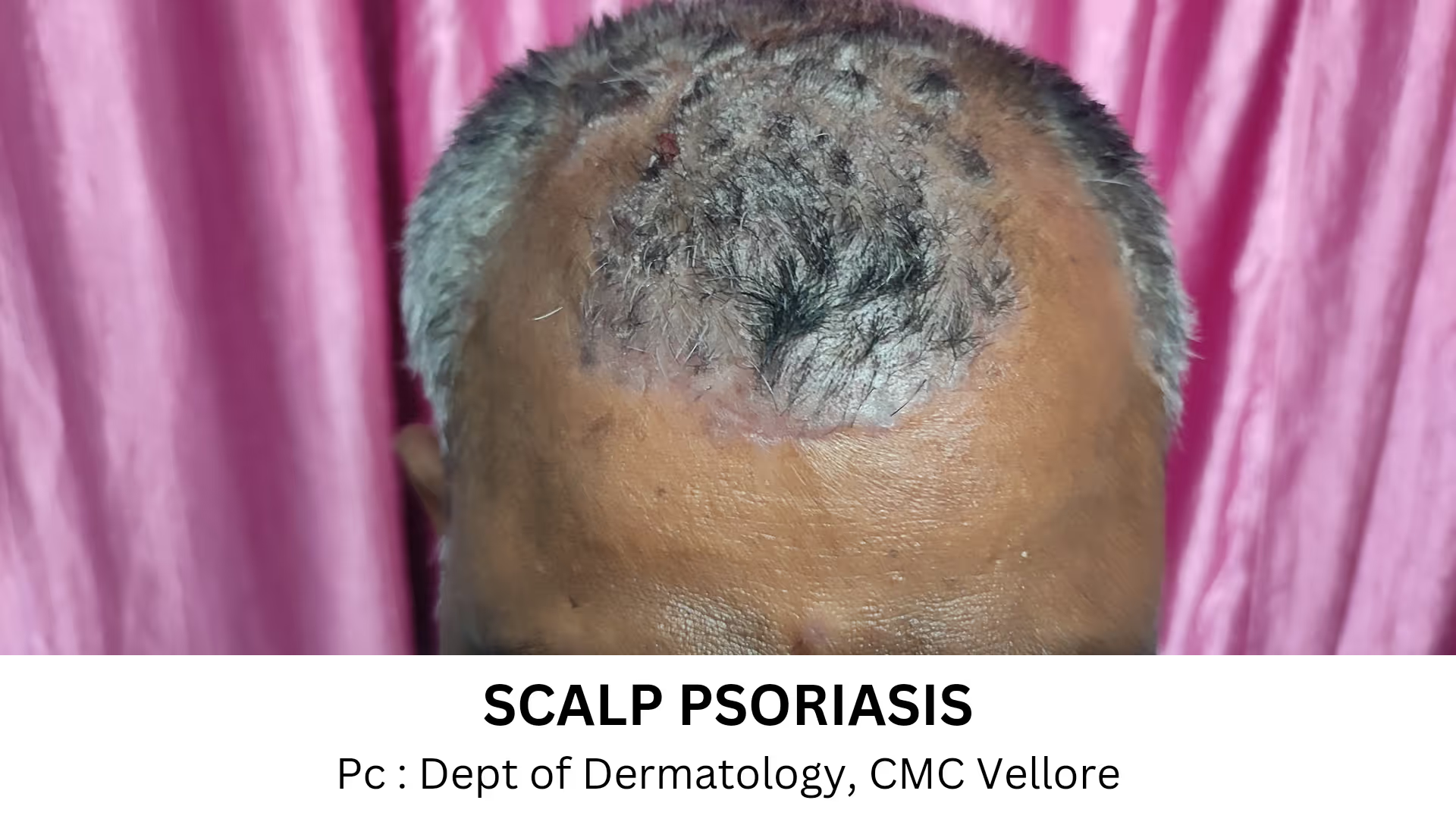
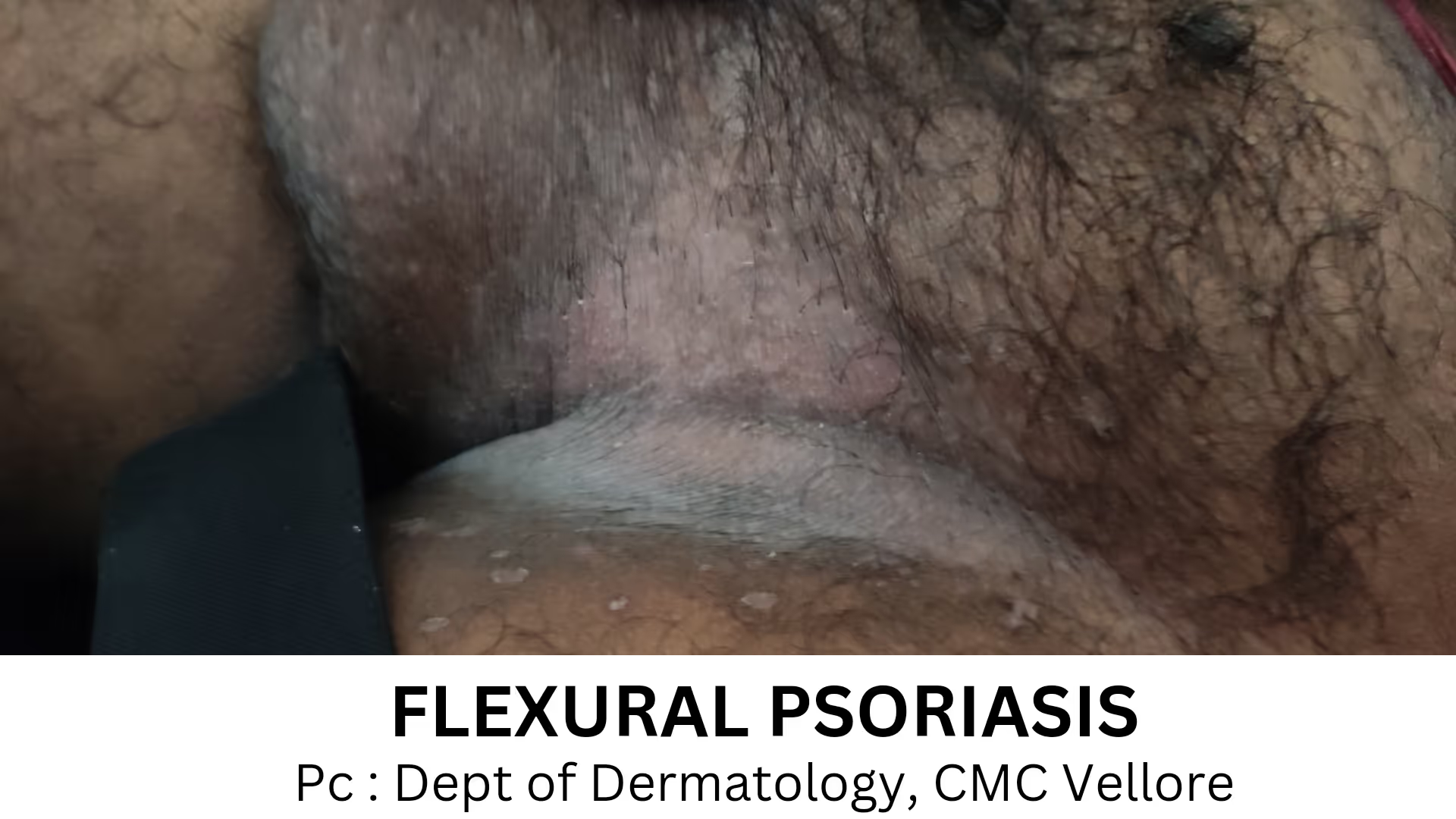
There are different types of psoriasis. Clinical picture varies on the body part involved, severity and the subtype of Psoriasis.
Psoriasis presents as well defined, raised, scaly, reddish, skin rashes mainly on arms, legs, palms, soles and scalp.
If psoriasis affects the hands and feet, painful fissures (cracks) can develop. They not only affect use of the hands, but can make the “sufferer” conscious of hands, and may avoid shaking hands etc. Walking gets affected if soles of feet are involved. Severe psoriasis on the body can be painful and distressing too.
Psoriasis may involve any site of the skin. Patients may have a single lesion or involvement of the whole body.
Few patients may have joint involvement in the form of pain, stiffness and swelling, particularly in the morning. Joints of hands are commonly involved.
If one gets psoriasis, he/she must consult a dermatologist.
Do not self-medicate or treatments from untrained physicians.
Improper or wrong treatments may make psoriasis unstable. It can delay recovery period.
Dermatologists help in diagnosis of or ruling out psoriasis. No laboratory tests are usually needed for diagnosis. Skin biopsy of a small sample of the skin tissue may be needed to confirm the diagnosis in doubtful cases.
Blood tests may be recommended to check out for co-existing diseases or when systemic medications are indicated.
Psoriasis, particularly moderate to severe psoriasis, is associated with an increased risk of anxiety, depression and harmful use of alcohol.
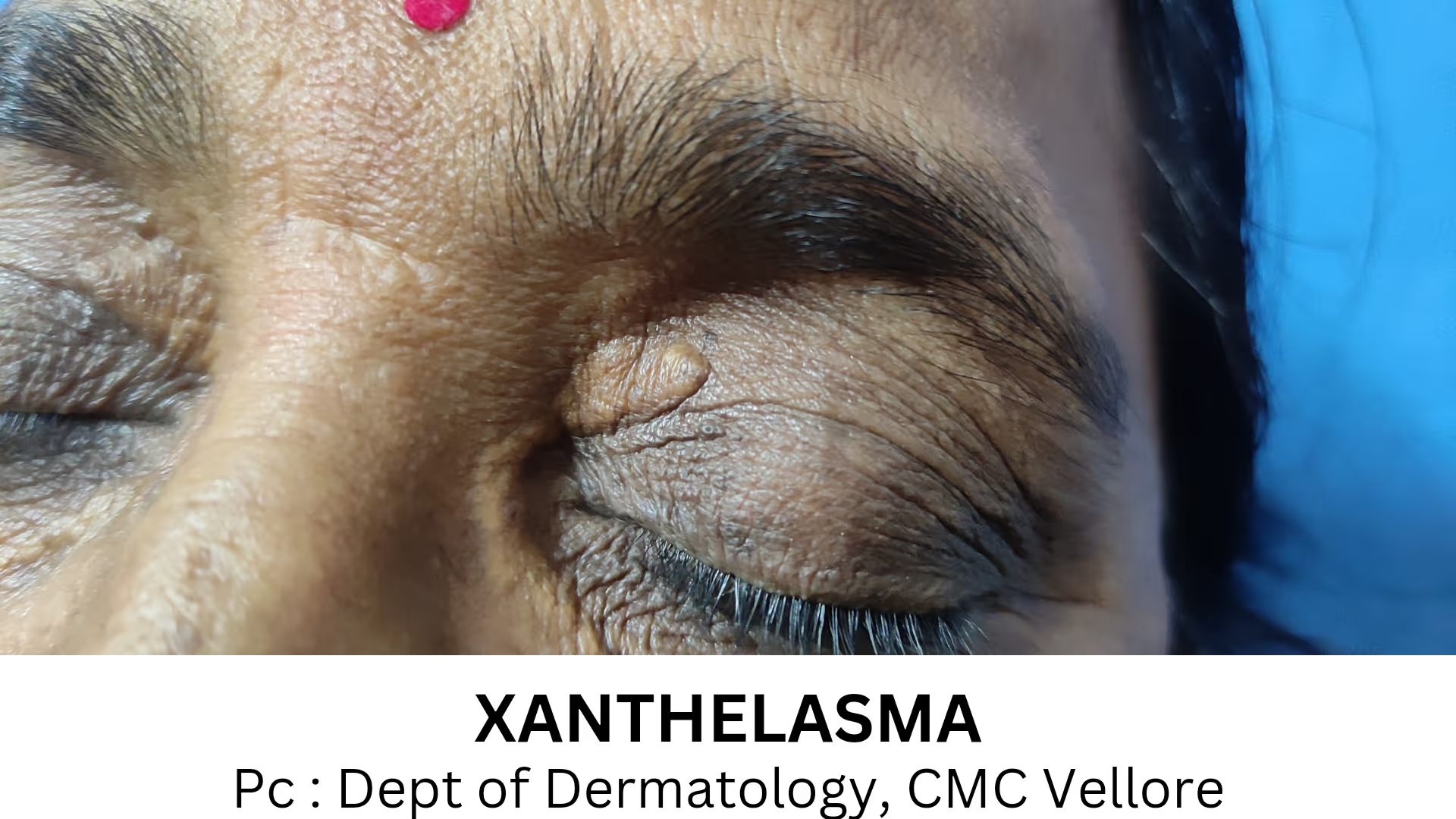
Psoriasis can also be associated with diabetes, obesity, high cholesterol and hypertension.
Early and timely interventions are needed.
Helps achieve remissions, meaning symptoms improve significantly and one can lead better quality of life
Can halt the progress of the condition.
Reduce symptoms such as itch and pain
Lessen the effects of related health conditions such as joint and heart disease, insulin resistance.
Keeping psoriasis under control tends to be an ongoing process. It requires appointments with your dermatologist. You’ll also need to follow treatment plan and learn what triggers your psoriasis. Once you know your triggers, you can avoid them. The treatment schedules vary for different types of Psoriasis. The Dermatologist will discuss the same with you and proceed accordingly. Patience, cooperation and regular follow up are essential for a good and long lasting remission, and also the progress to chronicity or a complicated disease.
There are different therapies available depending upon the severity of your disease. Creams and ointments can be used for limited disease, Systemic treatment (oral/ injectable medications) are required for severe disease or disease with co-morbidities (psoriasis associated with other diseases)
While there is no cure for psoriasis, there are more treatment choices than ever before. Several new treatments have become available in recent years. Researchers continue to study treatment options for psoriasis and make improvement
Psoriasis is an unpredictable disease. It is impossible to know who will have a remission (period of no disease) and how long it will last.
One may have no psoriasis symptoms (remission).
Sometimes, psoriasis may return, looking and feeling much like it did before (relapse).
Occasionally, psoriasis may return and be worse than before (rebound).
Do not be alarmed if there is relapse and rebound. It is a phase and symptoms will settle with appropriate care and treatment.
Since Psoriasis is a chronic condition, it is understandable that one may want to stop treatment by self. Always talk with your dermatologist before you stop treatment.
Your dermatologist can tell you whether you can stop the treatment abruptly or slowly. Sometimes, the best approach is to gradually switch to another treatment.
Disclaimer: This article is only for general patient information and is not intended for self medication. There is no legal liability of IADVL arising out of any adverse consequence to the patient. Subsequent to its use for self treatment of the disease images adjust for the depiction of the condition and is not to be used for any other purpose.
Explore articles in this section to gain a deeper understanding of various skin diseases and conditions. Each article provides detailed information on symptoms, causes, and treatment options, helping you to manage and address these dermatological issues effectively.

Painful swelling involving the hair is commonly known as boil or folliculitis. If it occurs more than three times in a year, it is known as recurrent folliculitis. when the infection is transmitted by direct skin contact.

Dandruff is a common scalp condition in which small pieces of dry skin flake off from the scalp and is usually associated with itching. The exact cause of Dandruff and Seborrhoeic Dermatitis is unknown.

Dermatophyte infection is a superficial fungal infection of skin, hair and nails. It is also known as ringworm. In Hindi it is termed as Daad and in Marathi it is termed as Gachkaran.